Cord Blood Research
Cord blood research became the focus of clinical research in the 1980s as it began to show promise in the treatment of blood diseases in children. Cord blood is an abundant supply of blood stem cells and is now used for treating over 80 diseases and disorders such as leukemia, lymphoma, aplastic anemia along with particular immune system and metabolic disorders. Cord blood transplants provide stem cells that grow new cells and are very similar to the better-known bone marrow transplant.
Importantly, cord-blood donors do not have to be entirely compatible with the recipient of the treatment. Cord blood stem cell treatment primary applies to children because one unit of cord blood most often lacks sufficient stem cells to treat an adult patient (approximately 50 to 100 ml). Generally, when cord blood is collected, the sample will provide enough stems cells to treat a child or small adult. The likelihood of ever needing cord blood is very low and the expense of storing a sample of cord blood privately are significant; however, there is new evidence everyday of the life-saving potential of cord blood treatment for certain patients and across a variety of disorders.
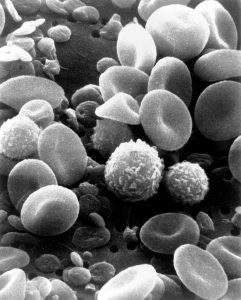
Specifically, umbilical cord blood is the blood that stays within the placenta as well as in the attached umbilical cord after childbirth. Cord blood contains each of the regular components of blood including red blood cells, white blood cells, platelets, and plasma. Umbilical cord blood provides a rich source of human stem and progenitor cells for patients requiring a hematologist cell transplant, which is more readily known as a bone marrow transplant . Research recently evaluating cord blood use among leukemia patients demonstrated that the rate of survival following the transplant was very similar amid patients who received transplants from donors who were unrelated. This is excellent news and the ability for cord blood to successfully provide transplants between unrelated and non-perfect match individuals is one of the most promising aspects of the area of cord blood research and application.
Since cord blood stem cells show such promise in various treatment outcomes across a variety of serious disorders, you can certainly understand why parents would want to consider private cord blood collection . Abundant in stem cells, cord blood is collected from the umbilical cord and placenta of volunteer donors right after delivery. Obtaining cord blood for donation is safe and painless for both mother and baby because it’s done after the umbilical cord is cut. Right after the birth of a baby, the umbilical cord is clamped and cut. To obtain a sample of cord blood, a second clamp is placed on the umbilical cord approximately 8 to 10 inches from the first clamp. Between the two clamps is where the blood sample is collected.
Umbilical cord blood collection is not part of routine obstetric care and is not medically indicated. Importantly, cord blood collection should not be performed in complicated deliveries. It is important for individuals considering cord blood collection to be informed. Obstetricians should assume that the awareness among pregnant women of cord blood donation and or storage is limited. Clinicians can help facilitate both communication and resources for parents considering the collection of cord blood during their baby’s birth. Obstetrician-gynecologists and other obstetric care providers may consult their governing bodies about current laws and practices surrounding cord blood collection and storage to become better informed.
As the interest, value and knowledge surrounding cord blood use increases, the same is true for the vast numbers of both private and non-private cord blood banks. HealthBanks Biotech Company Ltd., which is a company in Taiwan created the first facility to offer cord tissue storage back in 2008. The first private cord blood storage facility in the US was established in 2010. Similarly, the first public bank, New York Blood Center began in 1991. Since then the number of both public and private facilities have grown around the world and today exist in nearly every nation with approximately 500 cord blood banks operating worldwide.
Cord blood is either donated to a public cord bank and available for use worldwide by any patient and can be thought of as operating similar to the public venous blood banks or conversely, cord blood may be stored in a private cord blood bank for personal use by the donor or family. The cost of blood cord collection varies greatly; however, in the US cord blood banks may charge approximately $1,800 for the initial collection and processing. For those who want their own personal donation stored, private cord banks also charge an annual fee that is around $100 per year and again costs vary across facilities. The best case for choosing private banking is when there is a family history of any diseases or disorder that is currently treatable with cord blood, Cord blood units donated to public cord banks are collected under strict quality standards to provide the best possible results for transplant patients. Anyone can donate their baby’s cord blood to a public cord blood bank.
Cord blood collection and storage has developed into a potentially money-making business and as such requires careful consideration to ethical issues and strict regulatory policies. An act created in 2005 called the C.W. Bill Young Cell Transplantation Act was specifically created to provide funding for the continued development of a nationwide umbilical cord blood registry in the US. In some areas, the legislation requires physicians to raise the issue and resources about cord blood collection and storage including the option to give their baby’s cord blood to a public facility. In Canada, The Canadian Blood Services has obtained in excess of 11,000 samples across Canada and banked over 1400 units that are available as possible matches.
But should you bank, or donate? Consider the probability of utilizing the stem cells. Cord blood donation is a great idea particularly if the cord blood is stored in a bank for public use. Approximately 30% of all collected blood cord samples ultimately end up stored in a public cord blood bank. Parents considering private storage ought to carefully consider if there is a known family risk of a condition that is currently showing successful treatment with cord blood transplants. It is vitally important for parents to know when storing for a ‘just in case’ scenario that cord blood stem cells can contain already existing issues such as a premalignant cell change thus, cord blood is not always the answer when certain childhood diseases emerge. As reported by the National Marrow Donor Program, adequately stored cord blood may be viable approximately 10 years.
The area of cord blood research is rapidly developing. As such, it is important to ensure the processes surrounding cord blood research, collection, and storage continues to have strict regulations and ethical oversight. This also applies to both the public and private storage facilities. In addition, clinical care providers require education and on-going up to date information as do parents, who may be considering a public donation or private storage of their baby’s cord blood.
New and emerging areas of cord blood research and possible treatment for cord blood use in the areas of autism, brain injury, and other conditions continues along with new developments concerning the application for adult diseases such as cardiovascular issues is exciting. We look forward to continuing to monitor and stay informed about this exciting area of clinical research